Dan Leahy
Credit: Vivian Abagiu
Chair of the Department of Molecular Biosciences. Interviewed by Marc Airhart.
How do you see the department growing or changing in the next few years?
One big area of growth is structural biology, particularly cryo-electron microscopy, which is revolutionizing biology. We are just finishing construction on a new state-of-the-art cryo-EM facility, which will enhance many of our research programs. We will also start to collaborate with UT Austin’s new Dell Medical School. This will enrich our work by allowing us to go from model systems into disease systems, by giving us access to clinical samples and by exposing us to ideas and problems that may benefit from our basic-science perspective.
What kinds of research will the new cryo-EM facility enable?
Virtually any biochemical process – from copying DNA to building proteins to turning light into metabolism through photosynthesis –
involves molecules behaving and moving. And we want to see how those processes work. That can help us design better drugs, understand the causes of diseases and make better crops. It’s not a guarantee, but the more you understand at a molecular level, the more insight you can have to use biology to make human lives better.
Why is it useful to see molecules in detail?
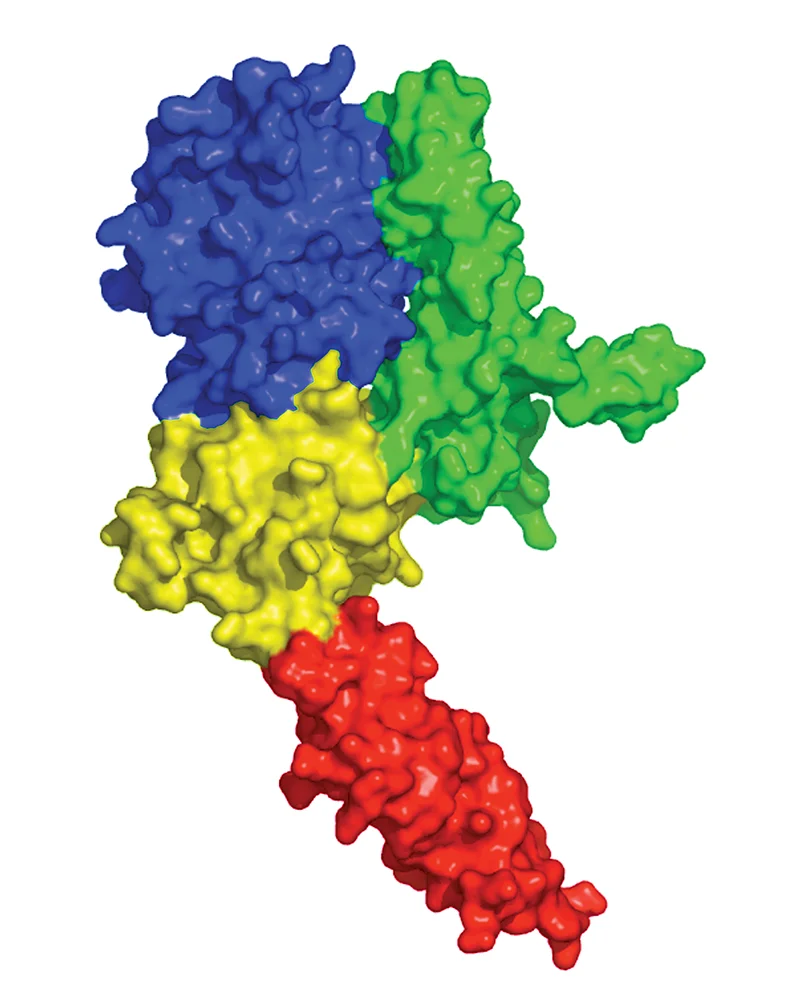
In structural biology, seeing is believing. A picture of a molecule helps us figure out how it works and how it interacts with other molecules to create living cells and tissues. It’s like taking apart a clock and studying all of the pieces to understand how it works.
What will you be studying with cryo-EM?
I study epidermal growth factor, an important receptor on cell surfaces involved in development and in healing skin after a wound. Tickle this receptor and the cells grow and divide, so mutated versions of the receptors are often involved in cancer. Consequently, many cancer drugs target these receptors. In my work, I try to see how the receptors and the drugs that target them work.
You played a role in getting a new breast cancer treatment into clinical use. Can you tell me about that?
A particularly aggressive form of breast cancer is caused by overexpression of a receptor called HER2. There was already a drug on the market called Herceptin that targeted HER2, but it didn’t work in some people, and in others, tumors often evolved resistance. Genentech had discovered another drug called Pertuzumab that also targeted HER2. We could see that the two drugs bound to different parts of HER2 and would inhibit its function in different ways. On the basis of this and other observations, Genentech decided to push Pertuzumab through clinical trials and received approval to market it. Now these two drugs are used together and, just as we suspected, they are more effective than Herceptin alone. By the way, Gail Lewis, a UT alumna and scientist at Genentech, played key roles in the development of Herceptin and Pertuzumab.